-
甲状腺癌是最常见的内分泌系统恶性肿瘤,占恶性肿瘤的1.1%。近年来,甲状腺癌的发病率呈逐年上升的趋势[1-2]。甲状腺乳头状癌(papillary thyroid carcinoma,PTC)是分化型甲状腺癌最常见的一种类型,容易复发,区域淋巴结的转移率较高。Lundgren等[3]认为TNM分期,包括远处转移和淋巴结转移是影响PTC患者预后的重要因素。目前,对于有肉眼可见的淋巴结转移患者,建议行区域淋巴结清扫术,但对于临床淋巴结阴性(clinical N0,cN0)期的患者是否行预防性中央区和(或)侧颈区淋巴结清扫仍存在争议[4]。
前哨淋巴结(sentinel lymph node,SLN)是区域淋巴组织引流原发恶性肿瘤的第一站淋巴结(一枚或数枚),其在淋巴直接引流通路上,并且最靠近原发灶,有可能最先受到原发肿瘤的侵袭,但并不一定是已经发生肿瘤转移的淋巴结。检测SLN能预测原发肿瘤次级淋巴结的状态,有利于早期发现颈部隐匿性的淋巴结转移,以避免不必要的淋巴结清扫对甲状旁腺和喉返神经造成永久性伤害[5]。SLN的检测是评估PTC患者淋巴结转移的一种微创技术。
目前,应用放射性示踪技术检测cN0期PTC患者SLN尚未广泛应用于临床,国际上暂无明确标准。本研究前瞻性地利用SPECT/CT对16例cN0期PTC患者的SLN进行探测,以评估放射性示踪技术对cN0期PTC患者SLN定位的价值。
HTML
-
选取2017年4月至11月在山西医科大学第一医院外科住院的PTC患者16例,其中男性2例、女性14例,年龄(47.0±8.4)岁,原发肿瘤直径(2.11±0.97) cm。纳入标准:所有患者术前均行甲状腺及颈部淋巴结超声检查,对超声怀疑有甲状腺恶性结节患者行细针穿刺活检,病理结果证实为PTC,并且临床检查及颈部淋巴结超声均未发现淋巴结转移。排除标准:孕妇及未满18岁的青少年、曾接受过颈部手术、颈部放疗、颈部淋巴结肿大、有甲状腺癌病史的患者。所有患者均在检查前签署了知情同意书。
cN0期患者的判定标准参考Kowalski等[6]提出的颈淋巴结临床评价标准,需同时符合以下条件:①临床触诊未发现肿大淋巴结或肿大淋巴结的最大直径<20 mm,质地柔软;②B超或CT检查未发现肿大淋巴结或肿大淋巴结最大直径<10 mm,或者最大直径为10~20 mm,但无中心性液化坏死、周边强化和淋巴结旁脂肪间隙消失;③缺乏影像学资料者以触诊为准。
颈部淋巴结分区依据美国耳鼻咽喉头颈外科学会的分区标准[7],分为颈中央区 (Ⅵ区)和颈侧区(Ⅰ~Ⅴ区)。Ⅰ区:包括颏下及下颌下区的淋巴结群;Ⅱ区:颈内静脉淋巴结上组;Ⅲ区:颈内静脉淋巴结中组;Ⅳ区:颈内静脉淋巴结下组;Ⅴ区:包括颈后三角区及锁骨上区淋巴结群;Ⅵ区:中央区淋巴结,为带状肌覆盖区域。
-
SPECT/CT为德国西门子公司 Symbia T16,配低能高分辨准直器。手持式γ探测仪为美国强生公司neoprobe2000型。超声扫描使用美国GE LOGIQ E9全数字化多功能彩色多普勒超声诊断仪。显像剂为99Tcm-硫胶体(99Tcm-sulfur colloid,99Tcm-SC),SC药盒由北京师宏药物研制中心提供,以85%的甲醇水溶液为展开剂,放射化学纯度≥92%。
-
手术前1天在超声引导下行甲状腺穿刺,于甲状腺肿瘤瘤体内注射约0.5 mL 99Tcm-SC(37 MBq),注射时应避免活动以确保注射部位准确,注射后按压注射部位10 min以避免局部血肿形成。注射显像剂后15~30 min行99Tcm-SC平面显像,2 h后行SPECT/CT显像(前后位)。显像时患者取仰卧位。平面显像时,能峰为140 keV,窗宽为20%,矩阵为128×128,放大倍数为1.0,采集10 min。SPECT/CT断层采集时,能峰为140 keV,窗宽为20%,矩阵为128×128,放大倍数为1.45。借助手持式γ探测仪于显像剂浓聚区相应的皮肤表面做标记,供术中参考。
SPECT/CT静态采集完成后,用同机X线行断层显像。图像重建采用迭代法,获得横断面、冠状面和矢状面的SPECT、CT以及两者的同机融合图像。
-
术中患者取仰卧位,在胸骨切迹上约两横指处顺皮纹方向作弧形领式切口,充分暴露甲状腺表面,确定甲状腺肿瘤位置,尽量保持甲状腺处于其解剖位置。在甲状腺全切术后,按照术前淋巴显像所显示的SLN数目与位置,利用γ探测仪探测甲状腺周围及颈部双侧Ⅱ~Ⅶ区放射性热点区域,切取放射性计数最高的淋巴结,将放射性计数为本底计数10倍以上的淋巴结定为SLN。切除所有有放射性摄取以及中央区没有放射性摄取的淋巴结,记录其数目及位置。将术中所有标本(甲状腺组织、SLN和非SLN)进行冰冻病理切片检查。
-
中央区以外,颈侧区SLN冰冻病理切片结果为阳性的患者同期行同侧颈部Ⅱ~Ⅵ区改良性清扫(保留颈内静脉、脊副神经和胸锁乳突肌);中央区SLN冰冻病理切片阳性和所有SLN阴性患者均在原颈前低领式切口下进行同侧颈择区性淋巴结清扫。颈部淋巴结清扫标本按分区整理后送常规病理切片检查。
1.1. 一般资料
1.2. 主要仪器和试剂
1.3. 检查方法
1.3.1. 术前SLN显像
1.3.2. 术中γ探测仪探测SLN
1.3.3. 手术及病理
-
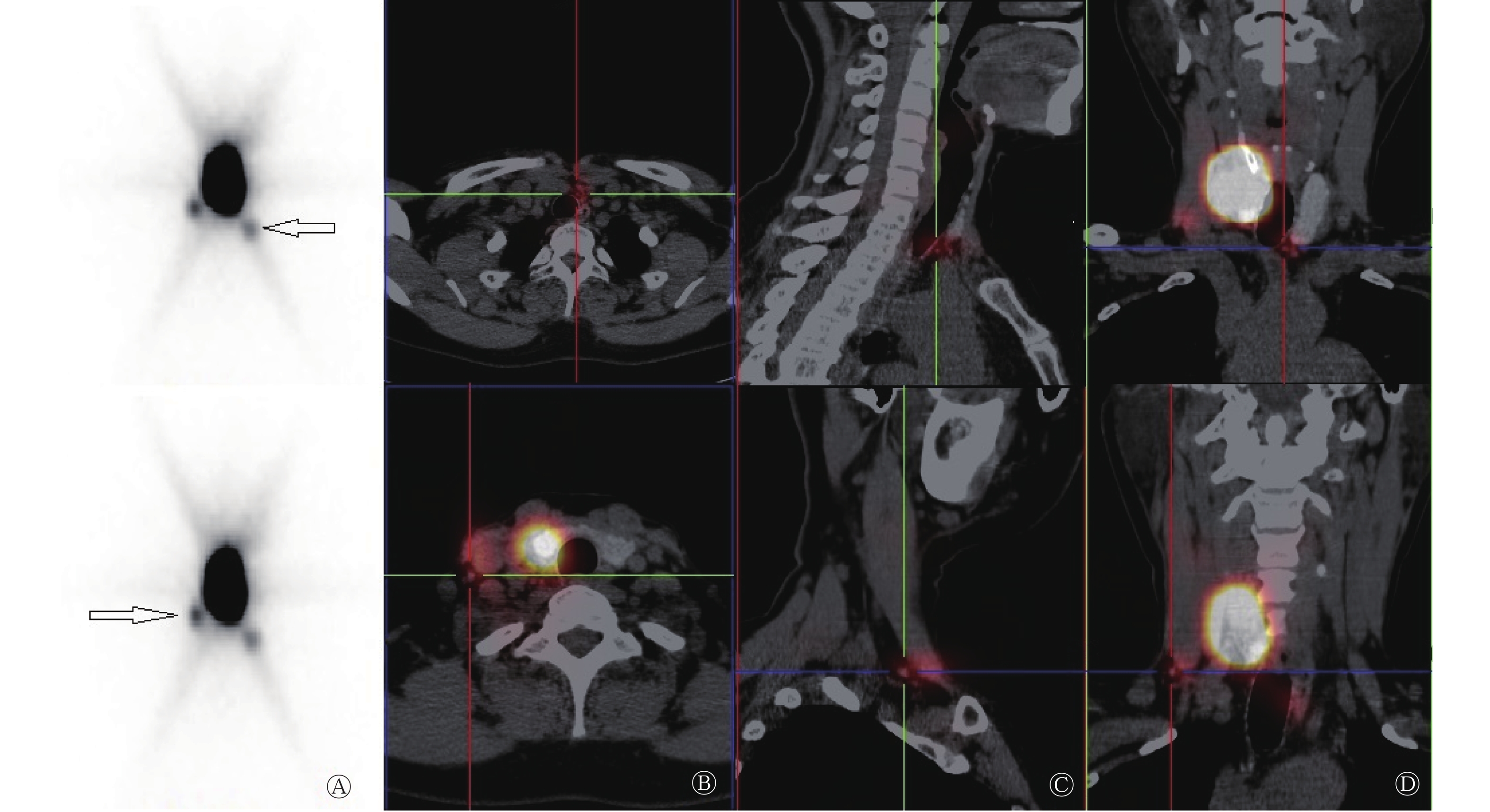
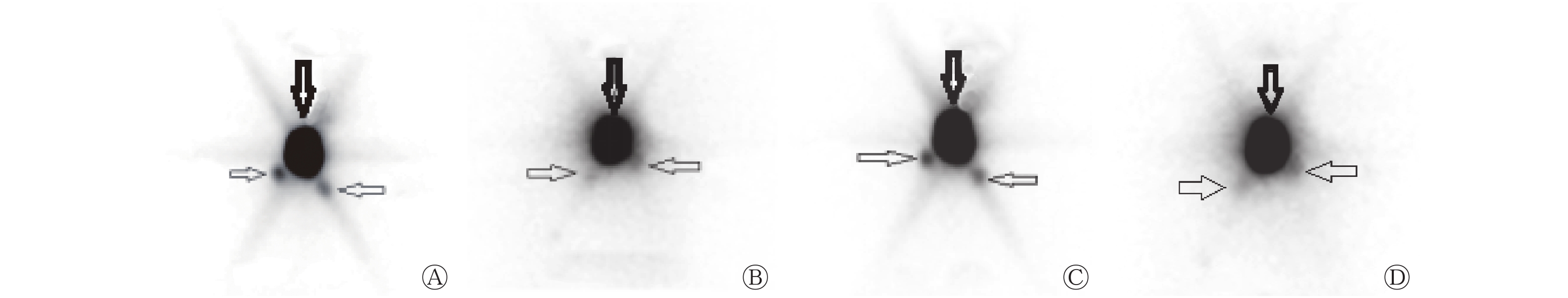
将距离注射点最近、出现时间最早、浓聚程度最高的放射性热点确认为SLN(图1)。
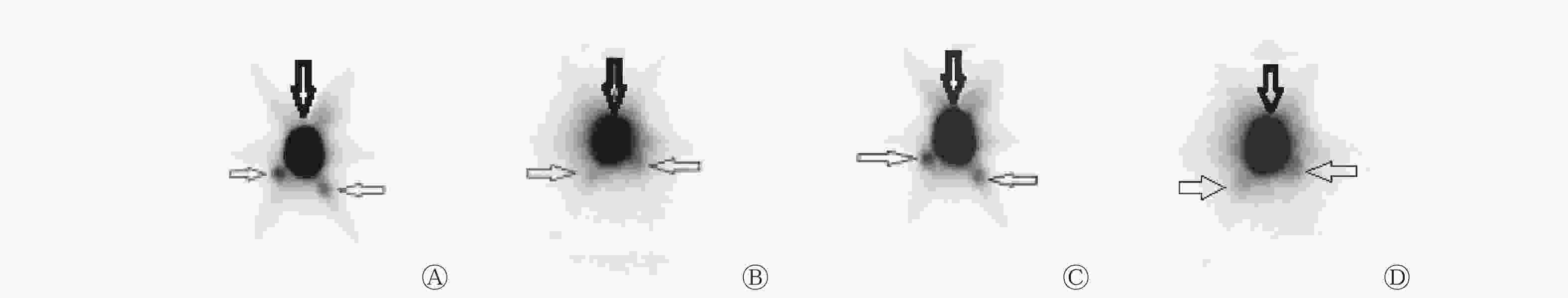
Figure 1. Preoperative sentinel lymph node planar images of a papillary thyroid carcinoma patient(female,54 years old)
SPECT/CT横断面、矢状面、冠状面断层融合显像见图2。
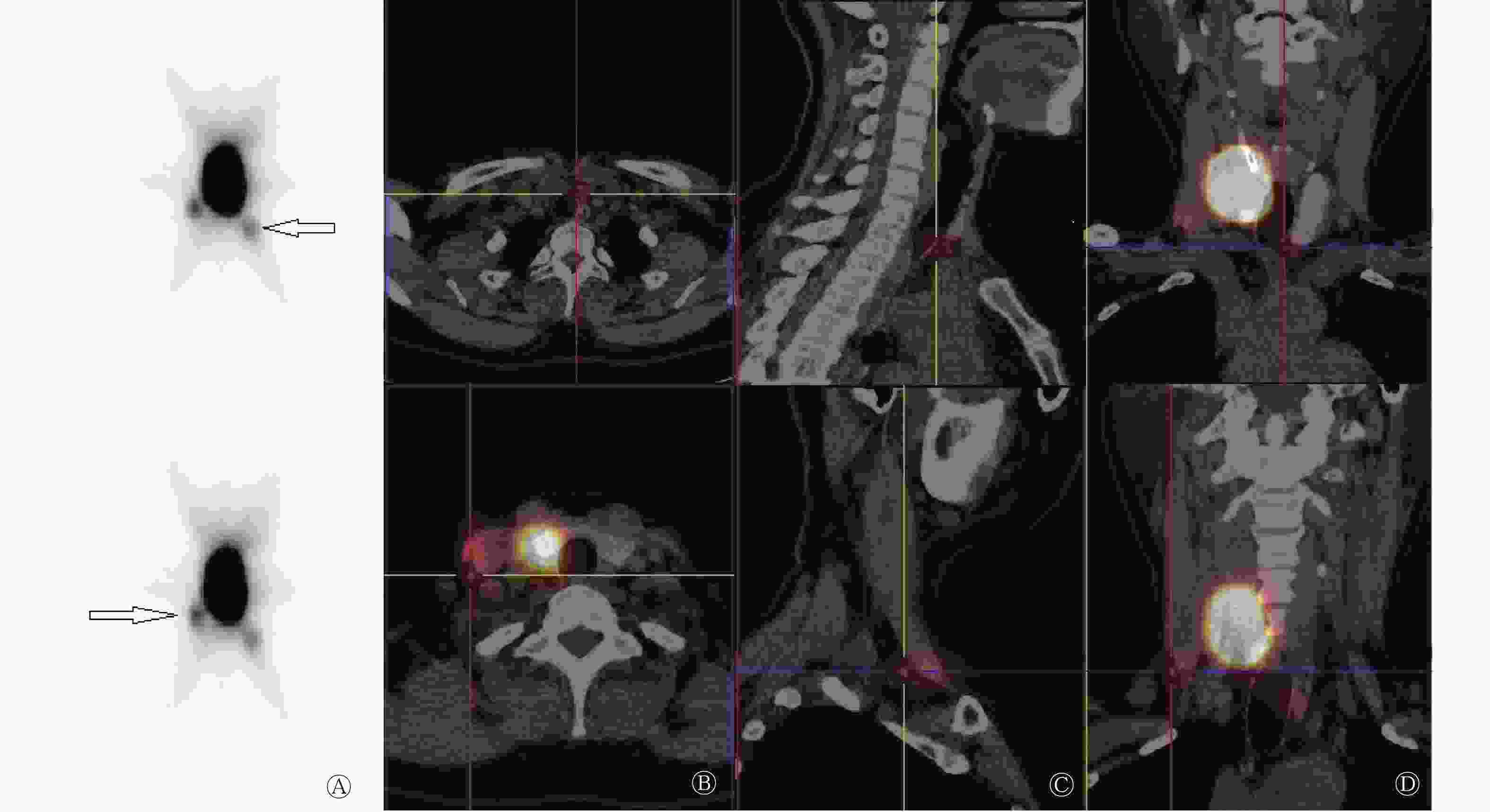
Figure 2. Preoperative sentinel lymph node SPECT/CT images of a papillary thyroid carcinoma patient(female,54 years old)
术前99Tcm-SC平面显像共检出SLN患者14例,检出率为87.50%(14/16)。99Tcm-SC平面显像共检出31枚SLN,SPECT/CT共检出35枚SLN。SPECT/CT检出1枚SLN者5例(31.25%,5/16),检出2枚SLN者1例(6.25%,1/16),检出3枚SLN者5例(31.25%,5/16),检出4枚SLN者2例(12.50%,2/16),检出5枚SLN者1例(6.25%,1/16)。
-
γ探测仪探测到13例患者的SLN,共计37枚,检出率为81.25%(13/16),有3例未探测到SLN(18.75%,3/16)。在探测到SLN的13例患者中,有3例探测到1枚(18.75%,3/16),1例探测到2枚(6.25%,1/16),5例探测到3枚(31.25%,5/16),3例探测到4枚(18.75%,3/16),1例探测到5枚(6.25%,1/16)。γ探测仪探测的SLN数目与SPECT/CT淋巴显像有4例不一致,12例一致,两种方法的一致率为75.00%(12/16)。
-
16例患者中,SPECT/CT检出14例有SLN。共检出SLN 35枚:其中位于Ⅵ区(中央区)的15枚;位于侧颈区共20枚,包括Ⅱ区的SLN 5枚、Ⅲ区的SLN 2枚、Ⅳ区的SLN 11枚、Ⅴ区的SLN 2枚。
将肿瘤部位分为上极、中极、下极、腺体。肿瘤位于上极者4例,共检出SLN 8枚:中央区4枚,有3枚转移;侧颈区4枚(Ⅲ区1枚、Ⅳ区1枚、Ⅴ区2枚),有3枚转移(Ⅲ区1枚、Ⅳ区1枚、Ⅴ区1枚)。肿瘤位于中极者3例,共检出SLN 7枚:中央区1枚,无转移;侧颈区6枚(Ⅱ区4枚、Ⅳ区2枚),有4枚转移(Ⅱ区2枚、Ⅳ区2枚)。肿瘤位于下极者4例,共检出SLN 14枚,中央区7枚,有7枚转移;侧颈区7枚(Ⅱ区1枚、Ⅲ区1枚、Ⅳ区5枚),有3枚转移(Ⅲ区1枚、Ⅳ区2枚);肿瘤位于腺体者3例,共检出SLN 6枚,中央区3枚,有3枚转移;侧颈区3枚,均位于Ⅳ区,有2枚转移。肿瘤位于下极,SLN最容易发生转移,中央区比侧颈区更常见,占转移总数的28%(7/25),占SLN总数的20%(7/35)。肿瘤位于下极,侧颈部Ⅳ区SLN检出数目相对较多,占侧颈区SLN总数的25%(5/20)。
-
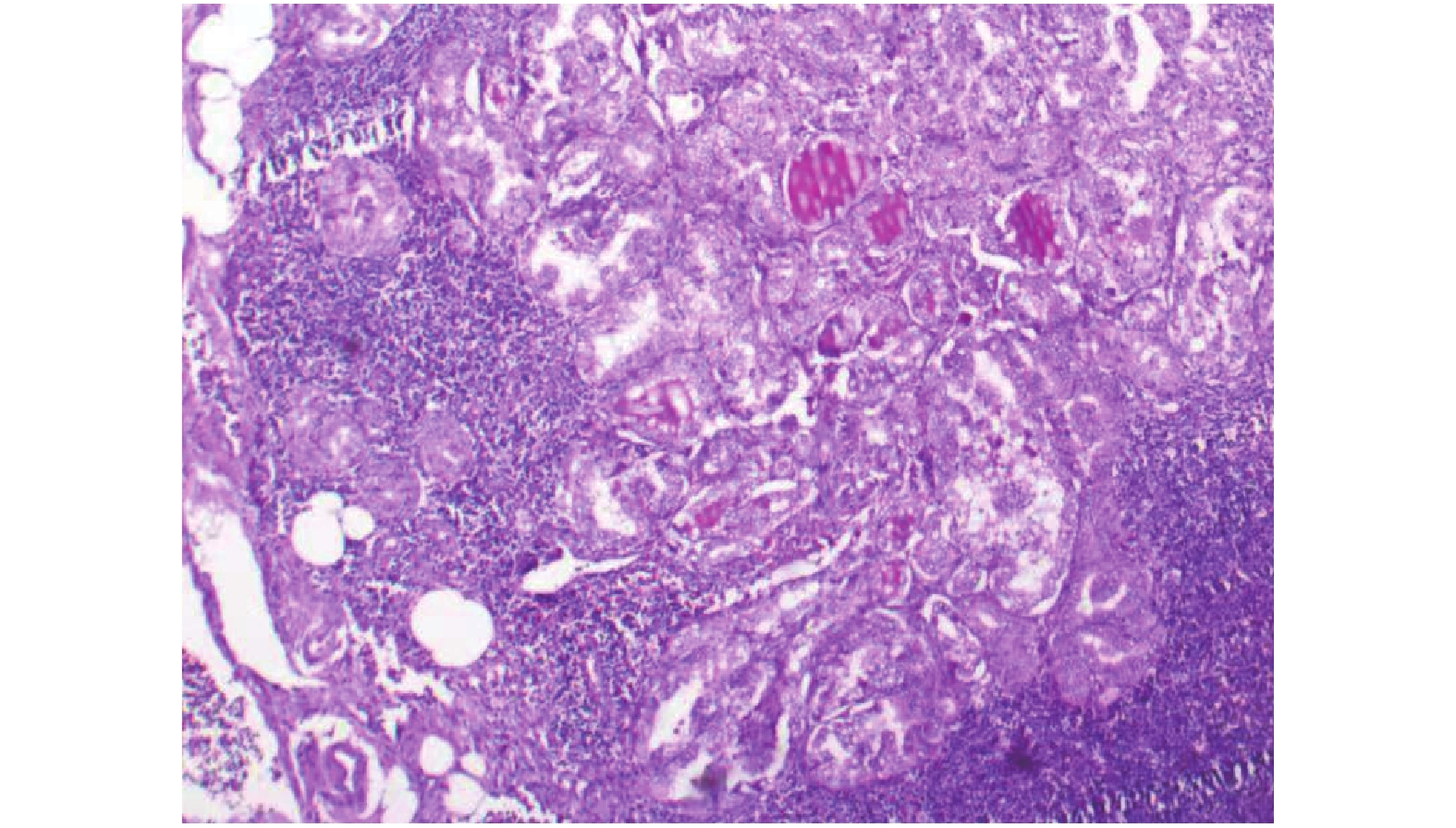
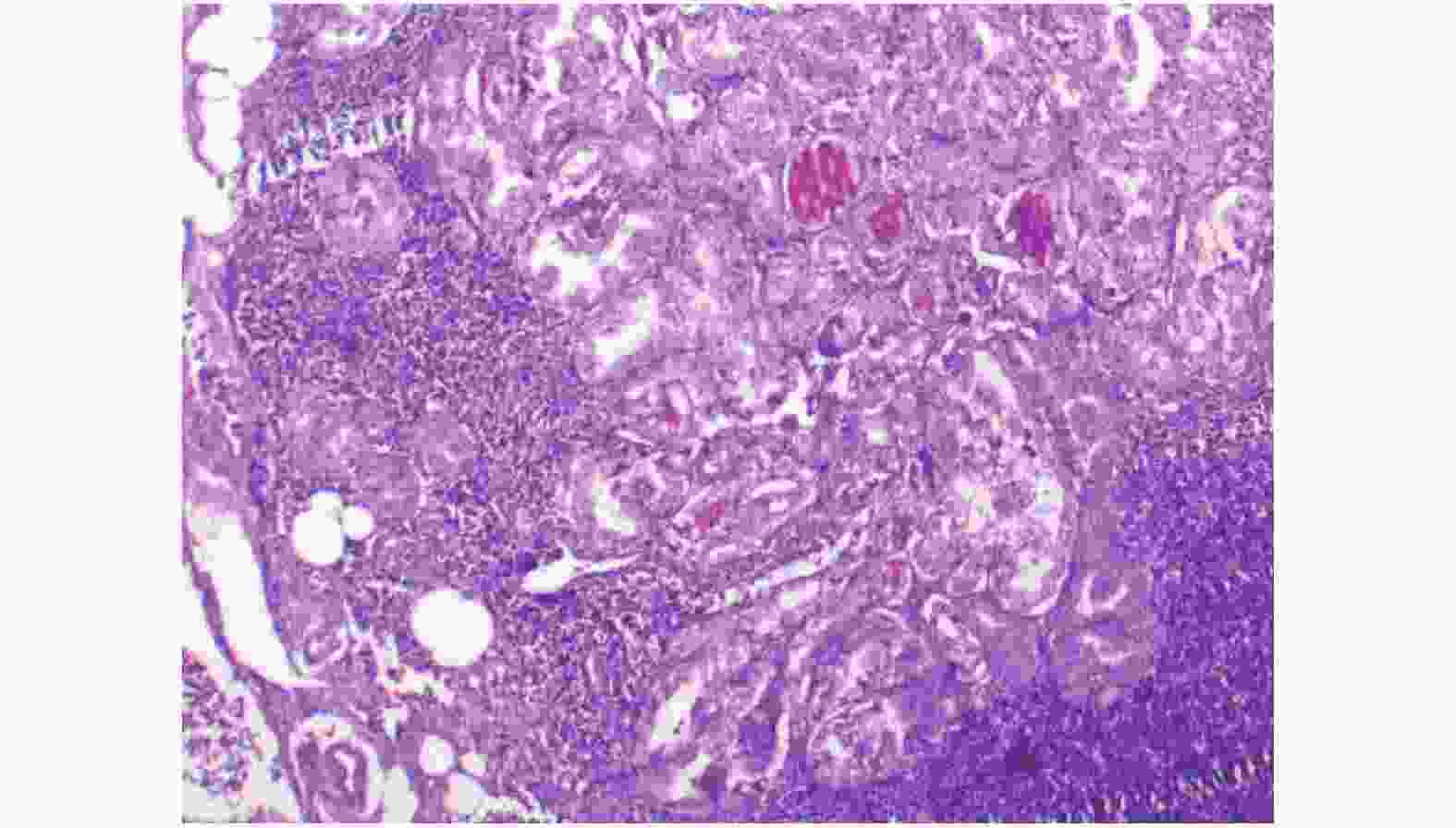
16例患者中,15例(93.75%)常规病理学检查有淋巴结转移(图3),其中SLN阴性2例。中央区SLN有13枚转移,阳性率为86.67%(13/15),侧颈区SLN有12枚发生转移,阳性率为60.00% (12/20)。SPECT/CT检测SLN的灵敏度、准确率、假阴性率分别为86.67%(13/15)、81.25%(13/16)、13.33% (2/15)。
2.1. 术前淋巴显像
2.2. 手持式γ探测仪的检测
2.3. SLN的分布情况
2.4. SPECT/CT淋巴显像与病理检查结果对照
-
PTC是分化型甲状腺癌最常见的类型,其隐匿性淋巴结转移率在70%~80%[8]。区域淋巴结转移与PTC的局部复发有显著相关性,以往观点认为颈部淋巴结转移不会影响PTC患者的总体生存率,但近年来有学者认为PTC区域淋巴结转移会降低患者的生存率,是影响预后的重要因素[9]。
目前,cN0期PTC患者的分期主要依靠临床检查和颈部超声检查。临床检查无法对颈部淋巴结进行精确定位,导致假阴性率高达30%[10]。超声检测淋巴结转移有较高的准确率,但特异度范围较大(52%~84%),主要原因可能是颈部存在其他隐匿性疾病[11]。由此可见,这两种方法证实有无淋巴结隐匿性转移的可靠性有限。
美国甲状腺协会指南建议,只有肿瘤细胞侵犯中央区淋巴结才能进行该区的淋巴结清扫,临床上未累及中央区淋巴结的原发肿瘤晚期(T3、T4期)或侧颈区淋巴结受累患者进行预防性中央区淋巴结清扫,对于T1期和T2期PTC患者,尚不推荐行预防性颈淋巴结清扫[12]。这可能会遗漏发生淋巴结转移的T1期、T2期患者,并扩大了未发生淋巴结转移的T3、T4期患者的手术范围。因此,临床上需要一种创伤小并能准确评估PTC患者颈部淋巴结状态、预测有无淋巴结隐匿性转移的技术。
SLN活检在1998年首次被应用于检测甲状腺癌淋巴结的转移情况,现在已成为cN0期PTC患者选择性淋巴结清扫的一种可供选择的方法[13-14]。SLN活检的主要方法:①生物染料示踪法;②放射性核素淋巴显像+ γ探针法;③两者联合法。与生物染料示踪法相比,淋巴显像+ γ探针法有明显优势:术前注射放射性药物,避免了术中清除病灶时破坏淋巴管使淋巴引流中断;中央区以外的SLN清晰显影,并能进行精确定位;甲状旁腺不显影,可避免误切除甲状旁腺[15]。
SPECT/CT将功能代谢影像与解剖结构影像实时融合。本研究中,SPECT/CT显像较平面显像多检出4枚SLN,提高了SLN的检出率,可能原因是SPECT/CT能发现平面显像上被邻近病灶掩盖的SLN,同时其可以鉴别体外污染、皮肤皱壁摄取显像剂的情况,从而降低假阳性率。
多个研究结果显示,术前SPECT/CT对SLN的检出率为79%~92%,术中γ探测仪对SLN的检出率为96%~100%[10, 16-18]。本研究中,术前SPECT/CT的SLN检出率为87.50%,而术中γ探测仪的SLN检出率为81.25%,稍低于96%。Portinari和Carcoforo[19]认为,影响术中γ探测仪SLN检出率的主要因素有显像剂注射的部位(瘤内或瘤外)和学习曲线效应等。由于本研究与多个研究[16, 20-21]均采用瘤内注射显像剂,所以受注射部位这一因素的影响较小。那么,在本研究中,学习曲线效应是否与术中γ探测仪的SLN检出率相关呢?结果显示,在第1例患者SPECT/CT显像中可见SLN显影,但γ探测仪未探及,并且前4例患者γ探测仪探测的SLN数目与SPECT/CT淋巴显像数目不一致,因此我们认为术中γ探测仪对SLN的检出率很可能与学习曲线效应有关。使用γ探测仪是逐步学习的过程,随着临床实践次数增多,熟练程度也随之增加,对SLN的检出也趋于准确。
本研究中共检出35枚SLN,中央区SLN检出率为42.86%(15/35),转移阳性率为86.67%(13/15);侧颈区SLN检出率为57.14%(20/35),转移阳性率为60.00%(12/20);与鄢丹桂等[22]研究结果相似(中央区SLN检出率为37.1%)。本研究通过术前淋巴显像+γ探测仪探测,检出SLN的准确率高达81.25%(13/16)、灵敏度为86.67%(13/15)、假阴性率为13.33%(2/15)。多项研究结果显示,通过对PTC患者行SLN活检的诊断准确率为86%~100%、灵敏度为67.0%~100%、假阴性率为0%~33.3%[22-26]。与以上研究结果相比,本研究对SLN的诊断准确率略低,考虑可能与样本量少有关,而灵敏度、假阴性率均与活检相似。本研究16例PTC患者中有2例行SPECT/CT淋巴显像时未发现SLN,但经病理学检查提示有淋巴结转移,导致诊断假阴性率为13.33%,分析原因可能有:肿瘤组织体积过大,引流淋巴管被肿瘤细胞侵袭,导致癌栓堵塞淋巴管,从而使淋巴引流方向改变,使有转移的SLN不能显示;老年患者淋巴组织萎缩被脂肪组织替代,使SLN难以显示;操作失误,将放射性显像剂注入肿瘤周围,导致显像剂溢出到周围组织。
Kaczka等[27]研究结果表明,绝大多数PTC患者的SLN分布于中央区,但也有部分出现在侧颈区[28-29]。本研究结果显示,肿瘤位于下极,侧颈部Ⅳ区检出SLN相对较多(25%,5/20)。4例患者有10枚SLN仅位于侧颈区,占28.57%(10/35),10枚SLN均发生转移。PTC患者颈部淋巴引流途径主要是以分区为导向,淋巴结转移一般首先出现在中央区。但临床上也发现部分PTC患者无中央区淋巴结转移而有侧颈区或上纵隔淋巴结转移,即淋巴结跳跃性转移,其发生率为2%~38%[30-31]。孙荣华等[32]研究认为,部分患者颈部淋巴结“跳跃转移”可能并非真正意义上的跳跃转移,而是PTC第一站引流淋巴结位于侧颈区。同时有研究证实肿瘤位置与PTC侧颈区淋巴结跳跃性转移有显著的相关性,如肿瘤位于甲状腺上极,其淋巴引流可能越过中央区直接流向侧颈区[29, 33]。本研究结果显示,当肿瘤位于上极,中央区与侧颈区发生转移的SLN数目一致,均占总转移数目12%(3/25)。
我们认为,若SLN为转移性淋巴结,这说明该区域淋巴结很可能也已发生转移,则需行该区域淋巴结清扫;如果SLN为阴性(经病理学检查证实无肿瘤转移),则说明该区域淋巴结尚未发生转移,暂不需行颈部淋巴结清扫。本研究结果显示,利用术前SPECT/CT淋巴显像,结合术中γ探测仪检测SLN,可以进一步准确定位SLN,预测cN0期PTC患者的颈部隐匿性淋巴结转移,指导术中选择合理的术式,以减轻手术负担,减少术后并发症。
本研究样本量有限,后续仍需扩大样本量进行前瞻性随机研究和长期随访,进一步证实术前SPECT/CT淋巴显像探测cN0期PTC患者SLN的临床价值。
利益冲突 本研究由署名作者按以下贡献声明独立开展,不涉及任何利益冲突。
作者贡献声明 胡珊负责病例的收集、辅助显像药物的准备及图像的采集分析、文献资料的查询及论文的撰写;杜芬负责图像的采集分析、文献资料的查询;白涛负责肿瘤穿刺及药物的注射;杨子瑶负责病例的收集;刘静负责手术及术中前哨淋巴结的定位;武晨负责病例收集及文献资料的查询;程艳、武志芳负责论文的指导和审校。







 DownLoad:
DownLoad: