-
炎性肌纤维母细胞瘤(inflammatory myofibroblastic tumor,IMT)是一种少见的具有复发潜能的间叶源性肿瘤,病理组织学上是由一种主要由分化的肌纤维母细胞性梭形细胞组成、常伴有大量浆细胞和(或)淋巴细胞的少见肿瘤[1]。肌纤维母细胞瘤的良恶性是一个具有争议的问题,目前认为肌纤维母细胞瘤为良性病变,仅有少数多灶性肌纤维母细胞瘤易于多处复发,甚至转移[2]。笔者分析1例临床确诊为恶性肌纤维母细胞瘤的18F-FDG PET/CT影像学表现及鉴别诊断,旨在提高对该病的认识。
-
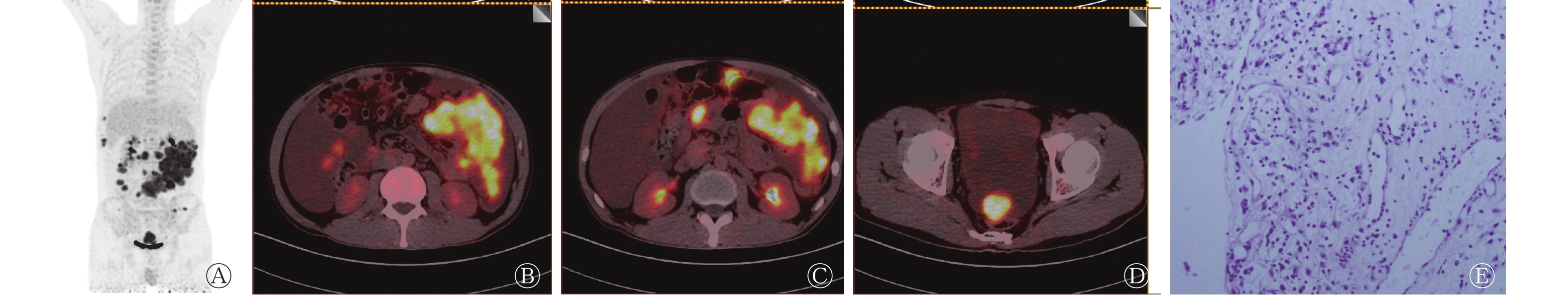
患者男性,34岁,20 d前无明显诱因出现腹部疼痛,呈阵发性,偶感胸闷,休息片刻可缓解,无呕血黑便、纳差乏力,近半月来体重增加15斤。当地医院就诊,行上腹部CT检查提示腹盆腔及网膜见多发散在大小不等结节灶和(或)团块影,盆腹腔大量积液,考虑恶性病变间皮瘤可能。在我院住院期间检查肿瘤标志物,结果发现糖类抗原CA125升高,为392.40(<35)U/mL,余正常。C反应蛋白升高,为147.00(<8.20)mg/L。于我院行18F-FDG PET/CT(289 MBq)检查示肝周、肠系膜、大网膜、左结肠旁沟及膀胱直肠间隙可见多发中低密度占位影,边缘尚清晰,伴18F-FDG显像剂异常浓聚,SUVmax=15.6。腹盆腔可见大量液体密度影,未见明显异常18F-FDG显像剂浓聚。PET/CT诊断考虑恶性病变(图1中A~D)。
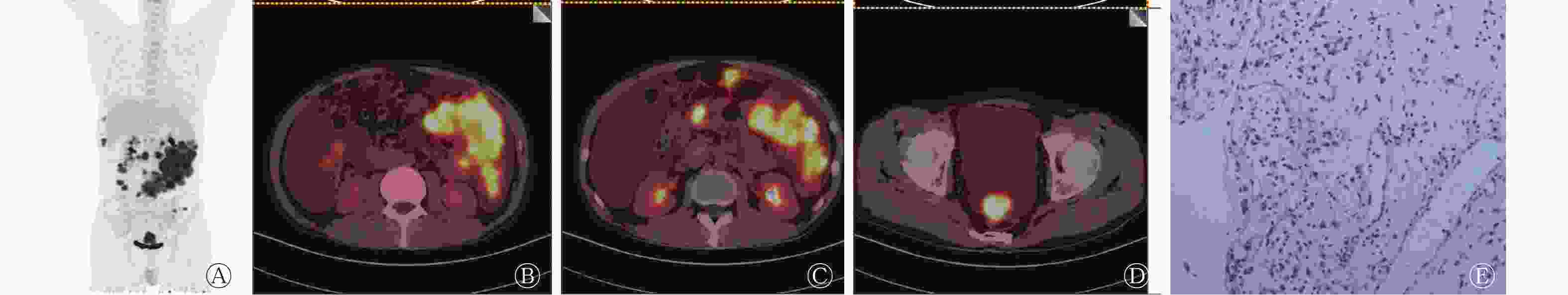
Figure 1. 18F-FDG PET/CT images and pathological images of malignant inflammatory myofibroblastoma(male, 34 years old)
于CT引导下行腹腔肿块穿刺活检。病理示(图1中E):穿刺组织条2根,长1.0~1.2 cm,直径为0.1 cm。腹腔肿块穿刺活检黏液背景下见散在梭形、短梭形、类圆形细胞,部分核仁明显,其间见血管和白细胞。结合形态学及酶标,首先考虑为IMT。免疫组化结果:肿瘤细胞CK(−),平滑肌肌动蛋白(−),Desmin(+),S100(−),Vim(+),CD34(血管+),CAM5.2(−),CD56(−),糖蛋白(少量+),人骨髓内皮细胞标记物(−),Syn(−)。
患者住院期间予腹水引流、止痛、加强营养等对症处理,因腹腔内多发病灶,考虑恶性病变,预后差,患者要求出院回当地医院。电话随访示PET/CT检查后1个月患者死亡。
-
2002年,IMT被世界卫生组织定义为由分化的肌纤维母细胞性梭形细胞组成,常伴大量浆细胞和淋巴细胞的一种间叶性肿瘤,包括浆细胞肉芽肿、组织细胞瘤、纤维黄色瘤、炎性肌纤维组织细胞增生、黏液样错构瘤、假性淋巴瘤、炎性纤维肉瘤和炎性假瘤等,尤以后者常见[3]。恶性肌纤维母细胞瘤在临床上比较罕见,Coffin等[3]认为腹腔内的IMT均有潜在恶性病变可能。
腹部肿瘤多表现为动脉期瘤内轻度片絮状强化,或边缘花环样明显强化,静脉期及延迟期强化范围持续扩大,强化程度无明显衰退。强化方式与瘤内组织成分比例有关,而恶性程度及预后转归与瘤细胞的核异型性有关[4]。从病理组织看,当梭形细胞出现异型性核,一种包涵体样核仁及较多核分裂时应视为恶性[5]。虽然肌纤维母细胞瘤的确诊主要依赖电镜,但根据特征性的组织形态学表现及其表达间变性淋巴瘤激酶的特点亦可作出病理诊断,间变性淋巴瘤激酶阳性的IMT有较高的复发倾向[6],该例患者病理取材穿刺组织,取材量有限,虽未发现典型的异型性核,但患者疾病进展迅速,PET/CT提示病灶弥漫分布,18F-FDG代谢明显增高,结合临床随访综合考虑为恶性。故对其良恶性判断,应根据临床资料、组织细胞学形态、随访情况等综合判断,而不仅仅局限于病理组织。亦有研究认为发生在鼻窦、鼻咽及腹膜后的IMT应视为恶性[7]。
IMT可发生于全身各处,病灶无特异性,该病例呈现为腹盆腔(以腹腔为主)多发大小中低密度占位,病灶边缘尚清,18F-FDG高代谢异常增高,主要考虑以下鉴别诊断。
1. 淋巴瘤:腹部和盆部的淋巴结是淋巴瘤常见的侵犯部位,包括腹膜后、肠系膜、髂窝等部位淋巴结,临床上常见脾脏和肝肿大。淋巴结多表现为密度均匀,淋巴结不易融合,少见坏死出血钙化。骨髓穿刺、淋巴结活检有助于明确诊断。
2. 间皮瘤:腹膜间皮瘤指原发于腹膜间皮细胞的肿瘤,间皮瘤易累及腹膜,恶性腹膜间皮瘤易于沿腹膜播散,常见腹水。增强扫描显示病灶实性成分明显强化。
3. 转移性腹膜肿瘤:腹腔脏器的癌瘤累及浆膜后,瘤细胞脱落,弥漫种植于腹膜、大网膜及肠系膜的表面,生长繁殖,被腹膜结缔组织包绕,形成大小不等的转移性结节,腹膜转移瘤引起血性腹水及脏器广泛黏连,导致患者死亡。
如考虑IMT诊断,即可避免不必要的根治性手术。通常可通过保守切除治愈,但边缘切除干净后仍有复发可能。不能切除的病变或复发性肺及头颈部病变可选择皮质激素治疗。采用大剂量皮质类固醇和非皮质类固醇抗炎药物治疗,部分患者症状消退。现有资料显示放化疗对IMT疗效不明显[8]。鉴于有恶性IMT远处转移和多年后复发的病例,有必要进行长期追踪随访。本研究中该例患者发病周期短,进展快,结合病理及免疫组化结果,符合恶性IMT表现,患者及家属拒绝进一步放化疗,短期内出现功能脏器衰竭死亡。此类疾病因良性多见,容易掉以轻心,重视程度不够,但少见致死性,尤其是发病速度如此迅速,值得深思。遇到类似患者应及早诊断,及早治疗,多发病灶手术无法切除者,应及早给与放化疗、激素冲击治疗。
利益冲突 本研究由署名作者按以下贡献声明独立开展,不涉及任何利益冲突。
作者贡献声明 张倩负责文献检索、论文撰写及修改;马超负责命题的提出和指导;吕中伟负责文章修改及润色。
Malignant inflammatory myofibroblastoma: 18F-FDG PET/CT imaging
- Received Date: 2019-01-04
- Available Online: 2019-11-01
Abstract: A case of malignant inflammatory myofibroblastoma was reported. The characteristics of the disease were analyzed using clinical symptoms, CT, 18F-FDG PET/CT examination, clinical diagnosis, pathological diagnosis, and prognosis. The understanding of this disease was deepened through literature review. The case was verified as malignant inflammatory myofibroblastoma. The disease progresses quickly and had low specificity. Diagnosis needed pathology and prognosis. Myofibroblastoma is mostly benign, and the incidence of malignant diseases is small. Once myofibroblastoma occurs, it is easy to misdiagnose. Thus, a combination of clinical, imaging, pathological, therapeutic, and prognostic considerations is needed.







 DownLoad:
DownLoad: