-
糖尿病胃轻瘫(diabetic gastroparesis,DGP)是糖尿病慢性并发症之一,主要临床表现为恶心、呕吐、饱腹感、腹胀、腹痛、厌食、嗳气等消化系统症状[1],DGP以排除机械性梗阻的条件下出现胃排空显著减慢为临床特点[2]。核素胃排空显像是一种在生理状态下判断胃排空功能的方法,具有无创、灵敏、可重复、符合生理、可定量等优点[3]。既往的放射性核素胃排空显像试餐种类及检查方法多样化,没有统一的判断标准,制约了其在临床的应用。我们应用99Tcm-DTPA液体试餐对正常志愿者行改良的放射性核素胃排空显像,以期为临床诊断胃排空功能损伤提供一个简便、准确的检查方法及相应的正常参考值和异常判断标准。在此基础上,进一步对糖尿病患者行胃排空显像,通过定量、定性分析,评估DGP发生率及其严重程度,指导临床诊疗。
HTML
-
选择潍坊医学院附属医院健康志愿者(对照组)55名,其中男性26名、女性29名,年龄18~65岁,平均年龄(52.3±10.4)岁,均无消化道器质性病变或相关手术史,无嗳气、反酸等消化系统不适的症状和体征。健康志愿者招募方案及该研究可行性均已通过潍坊医学院附属医院伦理委员会批准(志愿者招募证明书批件号:潍医附院伦理2015102001;批准证明书批件号:潍医附院伦理2015102002)。
为行前瞻性研究,使用简单随机抽样的方法,选取在潍坊医学院附属医院内分泌科门诊的2型糖尿病(诊断标准为1999年WHO制定)患者(试验组)100例,所有患者均无消化道器质性病变或相关手术史,近10 d未服用影响消化功能的药物。年龄25~70岁,平均年龄(57.8±9.8)岁。其中,无嗳气、反酸等消化系统症状者(试验1组)48例,包括男性22例、女性26例;有消化系统症状者(试验2组)52例,包括男性28例、女性24例。试验组和对照组两组年龄差异无统计学意义(t=1.65,P>0.05)。
所有研究对象均在检查前签署了知情同意书。
-
钼锝发生器由原子高科股份有限公司提供,经生理盐水淋洗得到Na99TCmO4液;DTPA(注射用亚锡喷替酸)由北京欣科思达医药科技有限公司提供;SPECT为GE公司生产的Infinia Hawkeye Ⅳ型双探头仪器,并配低能通用型准直器。
-
检查前0.5 h,取Na99TCmO4液1 mL,注入DTPA冻干品瓶中,将所得99Tcm-DTPA原液稀释至37 MBq/mL备用。取纯净水300 mL加温至37.5℃备用。检查前5 min,取37 MBq/mL的99Tcm-DTPA液1 mL,加入200 mL温纯净水中制备成所需液体试餐。该试餐使用方式为口服。
-
平卧前、后位显像:隔夜禁食8~12 h后,嘱受检者将液体试餐于1 min内饮完,随即加饮温纯净水100 mL,并立即仰卧于检查床上,SPECT两探头视野包含上腹部,即刻以1 min/帧×30帧的速度连续动态采集平卧前位及平卧后位影像。
坐立后位显像:平卧位检查结束3 d后,再次隔夜禁食8~12 h,嘱受检者将液体试餐于1 min内饮完,随即加饮温生理盐水100 mL,即刻以1 min/帧×30帧的速度连续动态采集坐立位后位影像。
-
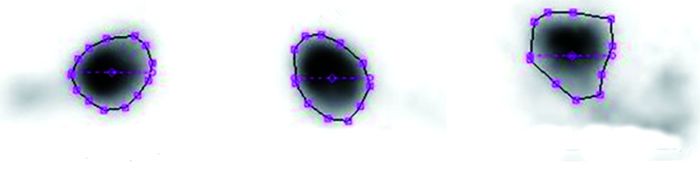
图像采集结束后,由两位副高级职称及以上医师分别在胃区勾画ROI,如图 1,两位医师勾画结果的放射性最大值和最小值相差分别在5%以内为有效ROI,经计算机处理生成时间-放射性曲线,对曲线分析后分别得到平卧前位、平卧后位及坐立后位胃半排空时间(gastric half emptying time,GET1/2)及30 min胃排空率(gastric emptying rate in 30 minutes,GER30min)。

Figure 1. Schematic for ROI selection in the images of gastric emptying in the lying anterior, lying posterior, and sitting posterior positions
GET1/2(min)=Cmax/2所对应横坐标数值
GER30min(%)=(Cmax-C30min)/Cmax×100%
公式中,Cmax表示胃区最大放射性计数,C30 min表示胃区30 min时的放射性计数。胃区时间-放射性变化曲线纵坐标表示计数率,横坐标表示时间(单位:min)。
-
使用SPSS17.0软件对所得数据进行统计学分析,计量资料以(x±s)表示,数据均符合正态分布且方差齐。对照组内采用成对样本t检验;对照组与试验组、试验1组与试验2组间采用独立样本t检验。P<0.05表示差异有统计学意义。
1.1. 一般资料
1.2. 99Tcm-DTPA液体试餐胃排空显像
1.2.1. 药物及设备
1.2.2. 99Tcm-DTPA液体试餐的制备
1.2.3. 胃排空显像
1.3. 图像处理与分析
1.4. 统计学分析
-
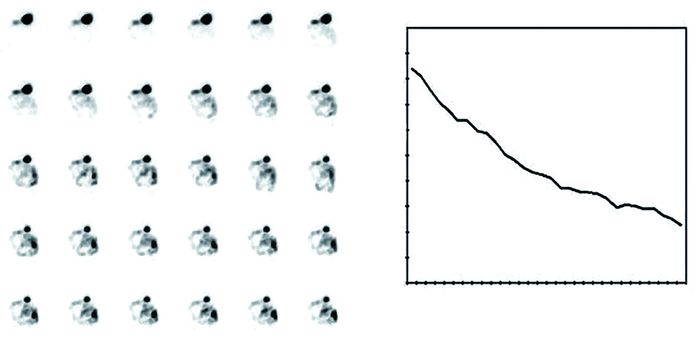
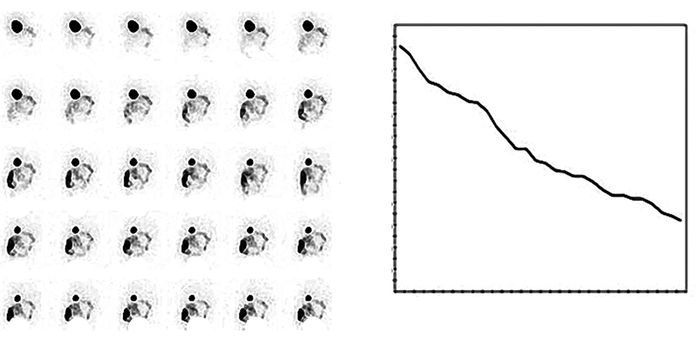
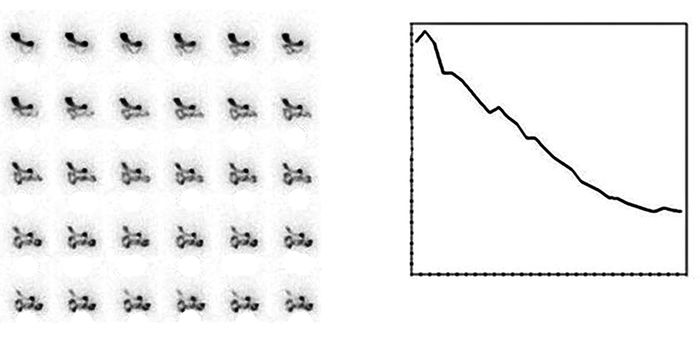
对对照组55名正常受检者平卧前位、平卧后位和坐立后位图像进行处理,分别得到胃区时间-放射性变化曲线(图 2~图 4)。分别计算每位受检者各体位的GET1/2和GER30 min,经统计处理后得到各指标的x±s及95%置信区间(表 1);正常对照组平卧前位、平卧后位及坐立后位GET1/2 95%置信区间分别为(8.41~17.11)、(7.35~16.67)、(5.91~13.47)min。对平卧前位和平卧后位、平卧后位和坐立后位GET1/2和GER30 min进行比较,差异均有统计学意义(t=5.35、11.20、-6.37、-9.77,均P<0.01)。其中,平卧后位及坐立后位检查易受脊柱影响,且坐立后位采集时受检者较难长时间保持体位不变,影响ROI的勾画。宜选用平卧前位采集,其GET1/2的95%置信区间上限为17.1 min。
参数 平卧前位 平卧后位 坐立后位 t值 P值 GET1/2/min 12.76±2.22 12.01±2.38a 09.69±1.93b 05.35 11.20<0.01 GER30min/% 80.14±7.12 82.54±7.33a 88.87±5.56b -6.37 -9.77<0.01 注:表中,GET1/2:胃半排空时间;GER30 min:30 min胃排空率。a是与平卧前位比较;b是与平卧后位比较。 Table 1. Comparison of GET1/2 and GER30min of different positions in the normal control group

Figure 2. Image of anterior gastric emptying in a normal person in lying position (1 min/frame) and its time-radioactive change curve
-
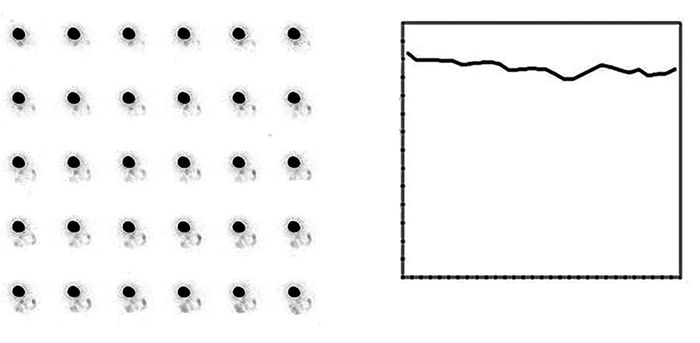
处理试验组的图像,得到平卧前位胃区时间-放射性变化曲线(图 5)。受检查时间限制,试验组糖尿病患者中存在GET1/2>30.0 min者,故不再将GET1/2作为参考指标。将对照组和试验组的平卧前位GER30 min进行比较,差异有统计学意义[(80.14±7.12)% vs.(70.16±12.86)%;t=6.22,P<0.01)],且试验组平卧前位GER30 min较对照组小。
-
将试验1组和试验2组平卧前位GER30 min进行比较,差异有统计学意义[(73.99±9.82)% vs.(66.66±14.34)%];t=3.01,P<0.05),其中,试验2组平卧前位GER30 min均值较试验1组小。
-
试验组患者胃排空功能相差较大,GER30 min跨度大,不能准确反映受检者胃排空功能,故将GET1/2作为评价糖尿病患者胃排空功能减退程度的指标。分别统计试验1组和试验2组GET1/2>17.1 min和GET1/2>30.0 min的例数并计算百分比(表 2)。有41%的糖尿病患者出现胃排空功能减退,其中9%的糖尿病患者胃排空功能重度受损。
组别 例数 GET1/2>17.1 min GET1/2>30.0 min 例数 比例(%) 例数 比例(%) 试验1组 048 14 29.17 2 04.17 试验2组 052 27 51.92 7 13.46 总计 100 41 41.00 9 09.00 注:表中,GET1/2:胃半排空时间。 Table 2. Degree of loss of gastric emptying tunction in patients with diabetes
2.1. 正常人不同体位胃排空显像比较
2.2. 对照组和试验组胃排空功能的比较
2.3. 糖尿病患者是否伴有消化系统症状对胃排空功能的影响
2.4. 糖尿病患者胃排空功能减退发生率
-
糖尿病发病率逐年增高,患者出现DGP后会严重影响生活质量。因此,临床上对DGP的早期诊治显得尤为重要。
既往检测胃排空功能的方法有以下几种:(1)X射线法,进食不能透过X射线的试餐后,测定不同时间点的胃排空情况,由于不能对胃内的残余钡量进行准确测定,故其临床应用受到限制[4]。(2)超声法,进食试餐后使用超声波检测胃的体积、形态的变化,根据相关计算方法确定胃排空的速率[5],但此法对肥胖受检者以及胃内有气体的受检者效果不佳,且较难定量。(3)MRI法,受检者进食Gd-DOTA(钆-铬合物化合物,为顺磁性造影剂)试餐后,用MRI进行扫描,即可显示消化道影像[6-7]。但此法不能获得连续数据,不能如实反映胃排空及运动功能的动态变化。(4)呼气试验,临床以13C作为示踪元素,根据转化为13CO2的量来间接推断胃排空功能,具有安全、方便的优点。但受受检者本身运动、疾病等因素的影响较大,且只能间接推断,缺乏权威性[5]。
放射性核素胃排空功能检测法是在短时间内进食放射性核素标记的试餐后,用SPECT进行动态连续数据采集,使用计算机对数据进行处理后得到胃区时间-放射性曲线,在生理状态下监测胃排空功能,是一种灵敏度高、重复性好、可定量、具有无创性且符合生理特点的检查方法[3, 8-9]。既往的放射性核素胃排空显像其试餐种类及检查方法多样化,没有统一的正常参考值判断标准,制约了其在临床的应用。我们选择99Tcm-DTPA液体试餐行改良的放射性核素胃排空显像,相对于固体试餐和固液混合试餐而言,具有试餐制备简单、放射性污染概率低、可缩短工作人员的受照时间、缩短受检者检查时间等优点。试餐量太多时受检者不能完全饮用,太少则不能如实反映受检者胃排空功能,为了不将液体试餐量作为观察变量,故经过多次试验,将本研究液体试餐量确定为统一适中量,即300 mL。
本研究通过应用99Tcm-DTPA液体试餐对胃肠功能正常的健康志愿者行改良的放射性核素胃排空显像,分别对健康志愿者平卧前位和平卧后位、平卧后位和坐立后位GET1/2和GER30min进行比较,差异均有统计学意义。其中,平卧后位及坐立后位检查易受脊柱影响,且坐立后位采集时受检者较难长时间保持体位不变,影响ROI的勾画。宜选用平卧前位采集,为临床胃排空功能测定选择了较好的体位。根据本研究结果可知,放射性核素液体试餐胃排空显像平卧前位GET1/2的95%置信区间为8.41~17.11 min,可以认为当GET1/2<8.41 min时为胃排空加快,当GET1/2>17.11 min时为胃排空功能减退。本研究中的图像采集时间为30.0 min,而部分实验组成员胃排空功能受损明显,故可以认为当GET1/2>30.0 min为胃排空功能重度受损。本研究结果为胃排空功能测定制定了较好的定量判断标准。
DGP发病率较高,其发病机制有以下几个方面:(1)自主神经病变,DGP患者内脏神经轴突发生脱髓鞘改变,使得迷走神经张力减低,胃排空延迟[10]。(2)高血糖症,高血糖既能引起神经病变,还能抑制胃肠运动,使胃窦收缩振幅频率减慢,幽门收缩引起胃排空延迟[11-12]。(3)胃肠道激素失调,糖尿病患者血中胃泌素水平升高[13-14],会导致胃排空延迟。国外流行病学调查结果显示,50%~76%糖尿病患者合并有DGP,且大部分患者并无明显消化道症状[1]。我们采用改良的放射性核素液体试餐对2型糖尿病患者行胃排空显像发现,有41%的患者出现了胃排空功能减退,与资料数据相近[1]。其中无消化系统症状的糖尿病患者,胃排空功能受损者占29.17%,胃排空功能重度受损者占4.17%;有消化系统症状的糖尿病患者,胃排空功能受损者占51.92%,胃排空功能重度受损者占13.46%。本研究结果显示,伴消化系统症状的糖尿病患者DGP的发生率更高,且更易出现重度胃排空功能损伤。
综上所述,99Tcm-DTPA液体试餐胃排空显像是一种简单易行、准确可靠的胃排空功能检测方法,根据GET1/2和GER30 min两个指标的计算结果能够对胃排空功能减退情况及程度作出判断[15-16],为临床诊疗提供了依据,可以作为临床检测胃排空功能的常规检查方法。本研究结果显示平卧前位胃排空显像受到的影响因素较少,并在此基础上制定了平卧前位胃排空功能正常参考范围及异常判断标准。通过液体试餐核素胃排空显像为糖尿病患者胃排空功能受损情况及受损程度进行良好判断,进而指导临床诊疗,具有较高应用价值,可在临床推广应用。











 DownLoad:
DownLoad: