-
乳腺癌已经成为全球女性癌症病死最主要的原因,其发病率居于女性恶性肿瘤首位[1]。乳腺癌是一种高度异质性的恶性肿瘤,在病理特征、临床表现和治疗疗效等方面均有明显的个体差异[2]。根据其免疫组织化学检查结果[如雌激素受体(ER)、孕激素受体(PR)、人表皮生长因子受体2(human epidermal growth factor receptor-2,HER-2)、细胞增殖核抗原(Ki67)的水平],可将乳腺癌分子分型分为Luminal A型、Luminal B型、HER-2过表达型、三阴性乳腺癌(triple negative breast cancer,TNBC)及其他特殊类型[3]。不同分子分型的乳腺癌具有不同的生物学特点,不同的生物学特点决定了其组织病理学改变不同,这也是影像表现的基础;同时乳腺癌不同的生物学特点也影响临床治疗方案的制定及疗效的评估[4]。本研究旨在探讨不同分子分型的乳腺癌在超声、MRI及乳腺X射线摄影检查中影像特征的差异。
-
回顾性分析2018年1月至2022年4月在惠州市中心人民医院就诊的212例女性乳腺癌患者的临床资料和影像资料,年龄(47.6±9.3)岁。根据其组织病理学和免疫组织化学检查结果分为4组:Luminal A型31例,年龄(49.2±10.8)岁;Luminal B型104例,年龄(46.1±8.9)岁;HER-2过表达型45例,年龄(49.6±10.1)岁;TNBC 32例,年龄(48.5±8.5)岁。纳入标准:(1)乳腺癌术后病理分子分型为Luminal A型、Luminal B型、HER-2过表达型及TNBC;(2)乳腺癌术前均行超声、MRI及乳腺X射线摄影等影像检查;(3)临床资料完整。排除标准:(1)乳腺癌术后病理分子分型不明确或为良性病灶;(2)患者术前已接受其他全身性治疗;(3)正值哺乳期或妊娠期的患者。所有患者均于检查前签署了知情同意书。本研究经惠州市中心人民医院伦理委员会批准(批准号:kyll2024008)。
-
所有患者在术前一周内完成超声、MRI及乳腺X射线摄影检查。应用荷兰Philips公司的Affiniti 50型和Affiniti 70型彩色多普勒超声诊断仪,探头频率为7.5~12 MHz。患者取仰卧位,上臂外展,以乳头为中心呈放射状扫查,发现病灶时进行十字形交叉纵横扫查,同时扫查双侧腋窝。
应用德国Siemens公司的Prisma 3.0T型MRI扫描仪,对患者行双乳及双侧腋窝MRI平扫及动态增强扫描。患者取俯卧位,双乳下垂。扫描序列及参数:采用Dixon fast序列进行横断面T2WI,重复时间4360 ms、回波时间81 ms、层厚4 mm、层间距0.8 mm、矩阵384×326;采用resolve序列进行横断面DWI,重复时间5510 ms、回波时间49 ms、层厚4 mm、层间距0.8 mm、矩阵204×101,b值为800 s/mm2。动态增强扫描对比剂采用钆特酸葡胺注射液(购自恒瑞医药),以高压注射器经手背静脉注射,剂量0.1 mmol/kg,流率2.0 ml/s,注射结束后用生理盐水冲管。采用T1高分辨各向同性容积激发序列进行动态增强扫描:重复时间4.21 ms、回波时间1.87 ms、层厚1 mm、层间距0 mm、矩阵352×352;先获取平扫图像,注入对比剂后连续采集5个时相,每个时相扫描117 s。
应用荷兰Philips公司的MicroDose SI型乳腺X射线机,双侧乳腺均行轴位(CC)及斜位(MLO)摄影,全自动曝光,必要时局部加压放大摄影。摄影条件为电压30~35 kV、电流15~20 mA。
-
分别由2位副高及以上职称的诊断医师进行独立阅片,观察并记录病灶的影像特征,意见不一致时经协商达成一致。在超声图像上提取病灶位置(左侧、右侧)、长径(≤20 mm、>20 mm~≤40 mm、>40 mm)、形态(不规则形、规则形)、边缘(光滑、模糊、分叶、毛刺或成角)、纵横比值(≥1、<1)、内部回声(均匀回声、不均匀回声)、后方回声(衰减或增强、无改变)、肿瘤内血流Alder分级(0或Ⅰ级、Ⅱ或Ⅲ级)。在MRI图像上提取乳腺实质背景强化(无或轻度、中度或重度)、强化形式(肿块型、非肿块型或点状)、强化特征(均匀强化、不均匀强化、环形强化)、动态增强曲线(流入型、平台型、流出型)、DWI弥散情况(高信号、等信号)。在乳腺X射线图像上提取乳腺腺体量(致密型、非致密型)、肿瘤内钙化情况(有钙化、无钙化)、钙化形态(点状、多形性或线样)等特征征象。分析并记录不同分子分型乳腺癌的影像特征以及患者的临床特征。
-
应用SPSS 23.0软件对数据进行统计学分析。符合正态分布的计量资料以
$\bar x\pm s $ -
由表1可知,不同分子分型乳腺癌患者的绝经情况、淋巴结转移情况差异均有统计学意义(均P<0.05),其中Luminal A型、Luminal B型及TNBC癌患者确诊时多处于未绝经时期;Luminal B型乳腺癌患者确诊时淋巴结转移阳性较高。
分型 年龄(岁, $\bar x\pm s $ 

绝经情况[例(%)] 淋巴结转移情况[例(%)] 已绝经 未绝经 阳性 阴性 Luminal A型(n=31) 49.2±10.8 9(29.0) 22(71.0) 12(38.7) 19(61.3) Luminal B型(n=104) 46.1±8.9 29(27.9) 75(72.1) 64(61.5) 40(38.5) HER-2过表达型(n=45) 49.6±10.1 24(53.3) 21(46.7) 18(40.0) 27(60.0) 三阴性乳腺癌(n=32) 48.5±8.5 14(43.8) 18(56.2) 13(40.6) 19(59.4) 检验值 t=0.113~1.037 χ2=10.345 χ2=10.026 P值 均>0.05 0.016 0.018 注:HER-2为人表皮生长因子受体2 Table 1. Comparison of clinical characteristics of female breast cancer patients with different molecular types (n=212)
-
由表2可知,不同分子分型的乳腺癌边缘、内部回声、肿瘤内血流Alder分级的差异均有统计学意义(均P<0.05)。Luminal A型乳腺癌肿瘤边缘多表现为模糊(图1A);Luminal B型和HER-2过表达型乳腺癌肿瘤边缘多表现为成角或毛刺(图1B、1C);TNBC肿瘤边缘多为分叶状(图1D)。Luminal A型、Luminal B型、HER-2过表达型及TNBC肿瘤内部回声多为不均匀回声,其中更多见于Luminal B型。Luminal A型和TNBC肿瘤内血流信号不丰富,Alder分级主要为0或Ⅰ级血流信号(图2A、2B);Luminal B型和HER-2过表达型乳腺癌肿瘤内多表现为丰富血流信号,即Alder分级主要为Ⅱ或Ⅲ级(图2C、2D)。乳腺癌肿瘤发生位置、长径、形态、纵横比值、后方回声差异均无统计学意义(均P>0.05,表2)。
分型 长径(mm) 位置[例(%)] 形态[例(%)] 边缘[例(%)] ≤20 >20~≤40 >40 左侧 右侧 不规则形 规则形 光滑 模糊 分叶 成角或毛刺 Luminal A型(n=31) 11(35.5) 11(35.5) 9(29.0) 18(58.0) 13(42.0) 31(100.0) 0(0.0) 5(16.1) 15(48.4) 6(19.4) 5(16.1) Luminal B型(n=104) 25(24.0) 58(55.8) 21(20.2) 51(49.0) 53(51.0) 95(91.3) 9(8.7) 8(7.7) 22(21.2) 30(28.8) 44(42.3) HER-2过表达型(n=45) 12(26.7) 21(46.7) 12(26.6) 23(51.1) 22(48.9) 44(97.8) 1(2.2) 1(2.2) 3(6.7) 18(40.0) 23(51.1) 三阴性乳腺癌(n=32) 11(34.4) 18(56.2) 3(9.4) 16(50.0) 16(50.0) 31(96.9) 1(3.1) 1(3.1) 4(12.5) 15(46.9) 12(37.5) χ2值 8.183 0.792 3.900 33.542 P值 0.225 0.851 0.272 <0.001 分型 纵横比值[例(%)] 内部回声[例(%)] 后方回声[例(%)] 肿瘤内血流Alder分级[例(%)] <1 ≥1 不均匀 均匀 衰减或增强 无改变 0或Ⅰ级 Ⅱ或Ⅲ级 Luminal A型(n=31) 20(64.5) 11(35.5) 26(83.9) 5(16.1) 18(58.1) 13(41.9) 19(61.3) 12(38.7) Luminal B型(n=104) 83(79.8) 21(20.2) 98(94.2) 6(5.8) 44(42.3) 60(57.7) 43(41.3) 61(58.7) HER-2过表达型(n=45) 37(82.2) 8(17.8) 37(82.2) 8(17.8) 16(35.6) 29(64.4) 16(35.6) 29(64.4) 三阴性乳腺癌(n=32) 27(84.4) 5(15.6) 23(71.9) 9(28.1) 13(40.6) 19(59.4) 21(65.6) 11(34.4) χ2值 4.756 12.283 3.983 10.699 P值 0.191 0.006 0.263 0.013 注:HER-2为人表皮生长因子受体2 Table 2. Comparison of ultrasonographic results of female breast cancer patients with different molecular types (n=212)
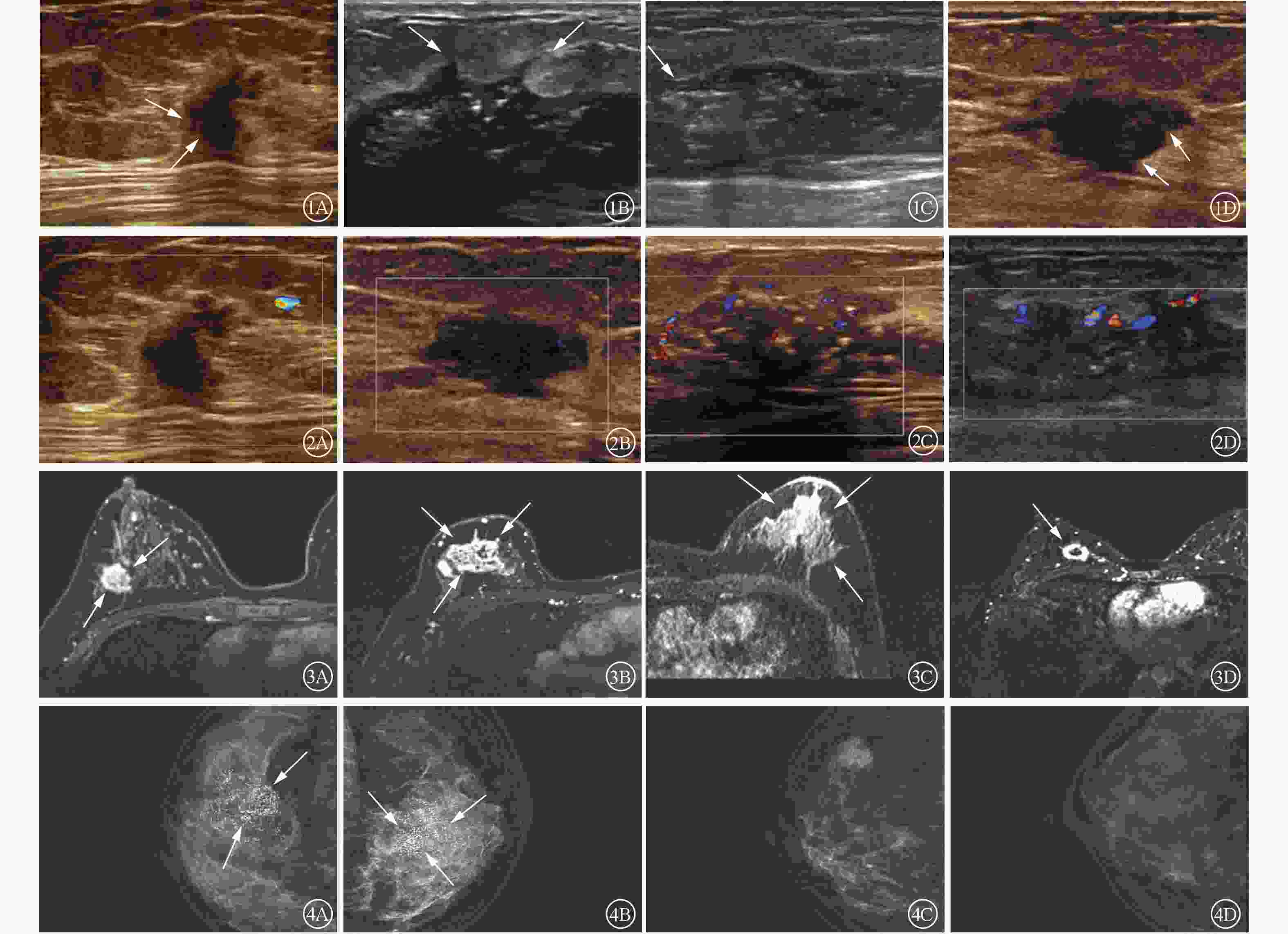
Figure 1. 2-Dimensional ultrasound imagings of breast cancer with different molecular types Figure 2 Color doppler ultrasound imagings of breast cancer with different molecular types Figure 3 MRI enhanced images of breast cancer with different molecular typesFigure 4 Mammography images of breast cancer with different molecular types
-
由表3可知,不同分子分型乳腺癌的肿瘤强化特征存在差异,且差异有统计学意义(P<0.001)。其中Luminal A型、Luminal B型及HER-2过表达型乳腺癌肿瘤强化特征以不均匀强化为主(图3A~C),而TNBC肿瘤环形强化的占比高于其他三者(图3D)。MRI乳腺实质背景强化、肿瘤强化形式、动态增强曲线、DWI弥散情况在不同分子分型乳腺癌中的差异均无统计学意义(均P>0.05,表3)。
分型 乳腺实质
背景强化强化形式 强化特征 动态增
强曲线DWI弥散
情况无或
轻度中度或
重度肿块型 非肿块型
或点状均匀
强化不均匀
强化环形
强化流入型 平台型 流出型 高信号 等信号 Luminal A型(n=31) 23(74.2) 8(25.8) 27(87.1) 4(12.9) 1(3.2) 27(87.1) 3(9.7) 1(3.2) 8(25.8) 22(71.0) 29(93.5) 2(6.5) Luminal B型(n=104) 69(66.3) 35(33.7) 80(76.9) 24(23.1) 19(18.3) 72(69.2) 13(12.5) 11(10.6) 18(17.3) 75(72.1) 99(95.2) 5(4.8) HER-2过表达型(n=45) 30(66.7) 15(33.3) 35(77.8) 10(22.2) 13(28.9) 27(60.0) 5(11.1) 0(0.0) 14(31.1) 31(68.9) 45(100.0) 0(0.0) 三阴性乳腺癌(n=32) 23(71.9) 9(28.1) 28(87.5) 4(12.5) 6(18.8) 12(37.5) 14(43.7) 0(0.0) 8(25.0) 24(75.0) 32(100.0) 0(0.0) χ2值 0.926 2.871 30.142 12.176 2.709 P值 0.819 0.412 <0.001 0.058 0.439 注:MRI为磁共振成像;DWI为弥散加权成像;HER-2为人表皮生长因子受体2 Table 3. Comparison of MRI results of female breast cancer patients with different molecular types (n=212, cases (%))
-
由表4可知,不同分子分型的乳腺癌肿瘤内钙化情况的表现差异有统计学意义(P=0.022),其中Luminal B型及HER-2过表达型乳腺癌肿瘤内多伴有钙化(图4A、4B),而Luminal A型及TNBC肿瘤内多无钙化(图4C、4D)。Luminal A型与Luminal B型乳腺癌肿瘤内钙化形态以点状钙化为主,HER-2过表达型及TNBC肿瘤内钙化形态以多形性或线样为主,差异有统计学意义(P=0.008);乳腺腺体量在不同分子分型的乳腺癌中差异无统计学意义(P=0.096,表4)。
分型 腺体量 肿瘤内钙化情况 钙化形态 致密型 非致密型 有钙化 无钙化 点状 多形性或线样 Luminal A型(n=31) 25(80.6) 6(19.4) 12(38.7) 19(61.3) 10(83.3) 2(16.7) Luminal B型(n=104) 88(84.6) 16(15.4) 63(60.6) 41(39.4) 44(69.8) 19(30.2) HER-2过表达型(n=45) 30(66.7) 15(33.3) 31(68.9) 14(31.1) 14(45.2) 17(54.8) 三阴性乳腺癌(n=32) 26(81.3) 6(18.7) 14(43.8) 18(56.2) 5(35.7) 9(64.3) χ2值 6.346 9.627 11.792 P值 0.096 0.022 0.008 注:HER-2为人表皮生长因子受体2 Table 4. Comparison of mammography results of female breast cancer patients with different molecular types (n=212, cases (%))
-
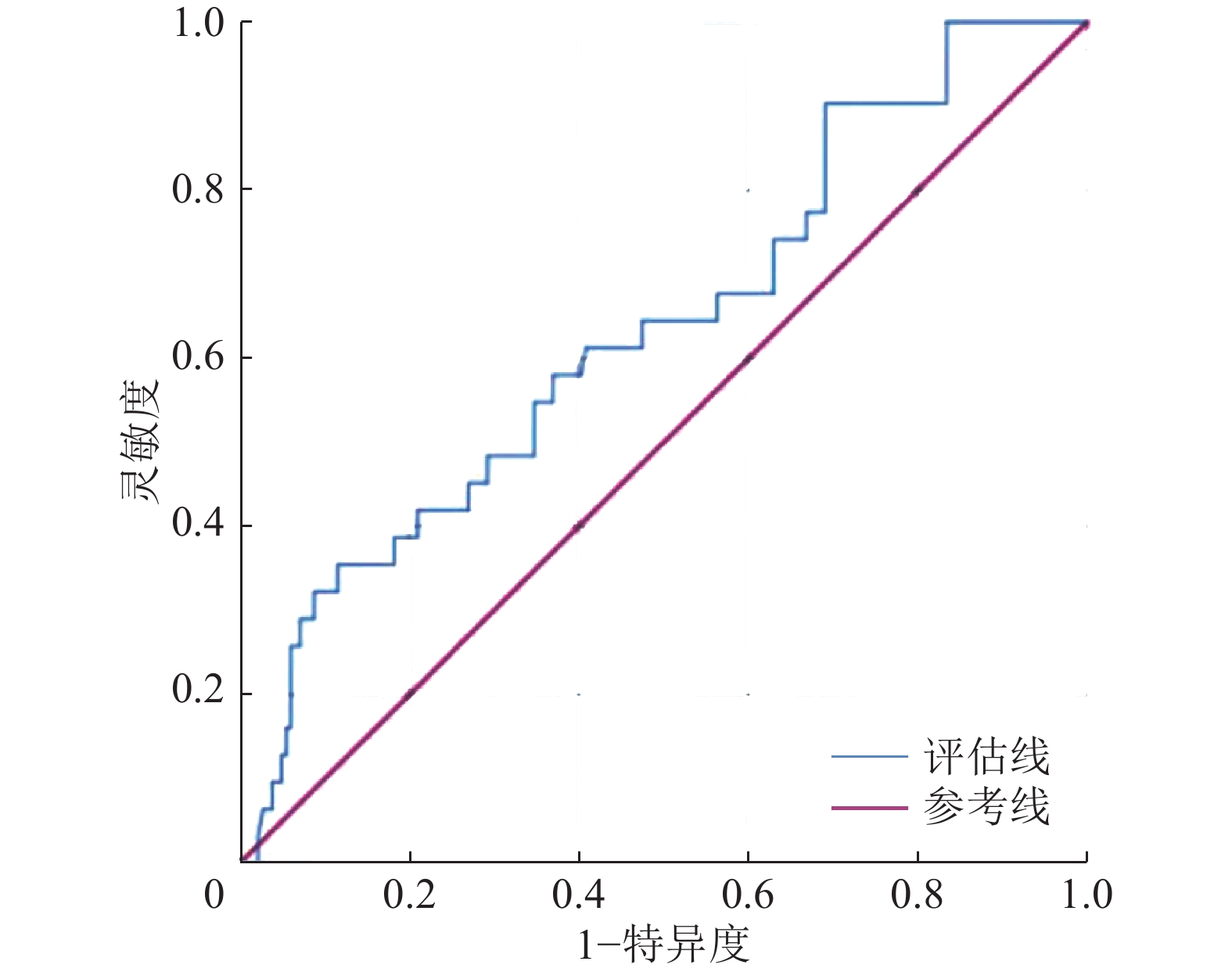
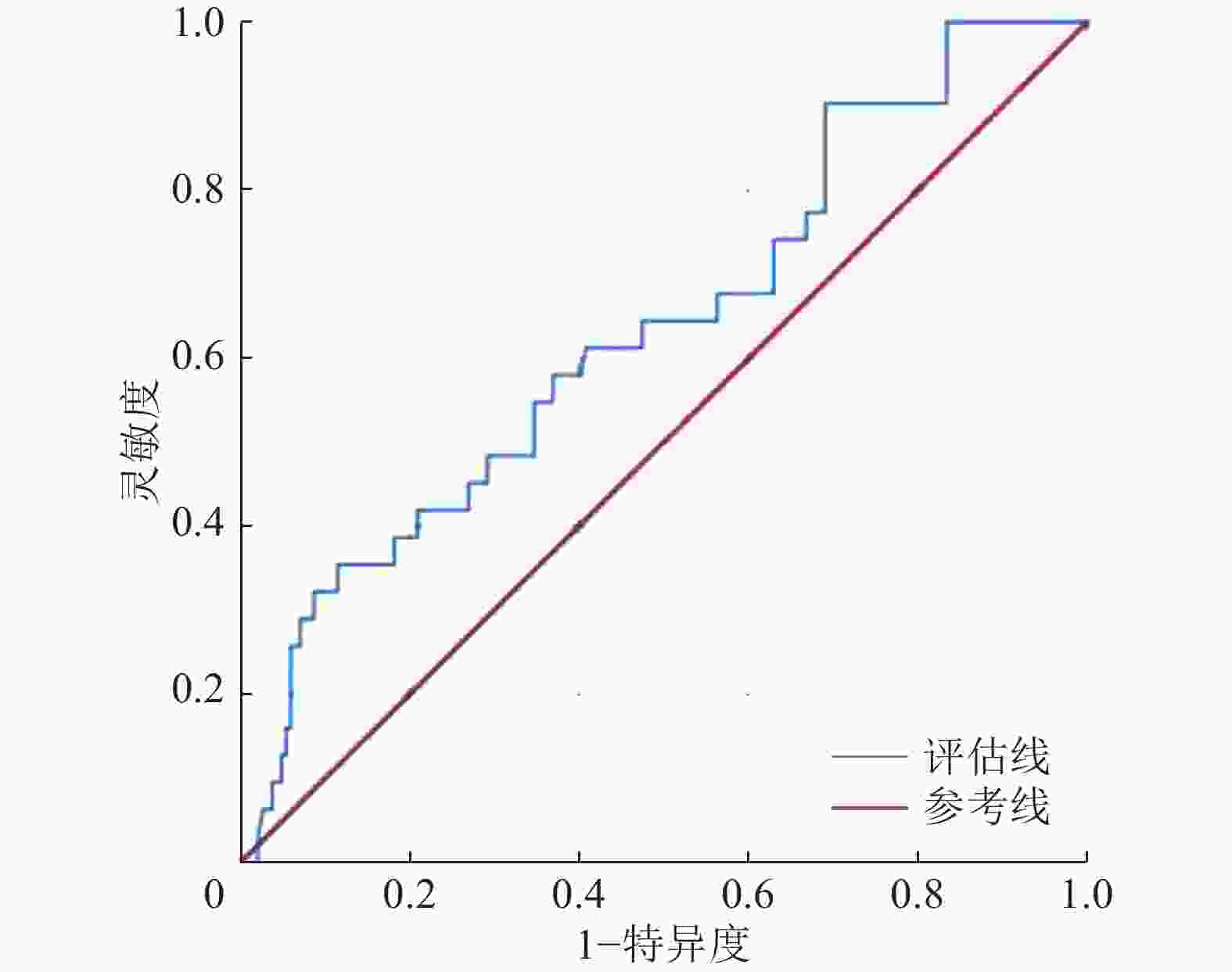
将单因素Logistic回归分析中差异有统计学意义的变量进一步纳入多分类有序Logistic回归分析,结果显示,患者绝经情况与乳腺癌肿瘤边缘可作为乳腺癌分子分型的独立预测因子(B=0.729、0.775,OR=7.053、23.696,95%CI:0.193~1.267、0.463~1.087,P=0.008、<0.001),AUC为0.635(95%CI:0.528~0.742),这表明患者绝经情况与乳腺癌肿瘤边缘情况对乳腺癌分子分型具有一定的诊断效能(图5)。
-
不同分子分型乳腺癌的治疗方式不同。本研究探讨了超声、MRI和乳腺X射线摄影特征对不同分子分型乳腺癌的诊断价值,以期为乳腺癌的治疗提供一定的临床支持。
本研究中,患者的发病年龄对乳腺癌分子分型的鉴别无统计学意义,患者的绝经情况对乳腺癌分子分型的鉴别有统计学意义。Luminal B型和TNBC患者发病时尚未绝经的可能性高于Luminal A型和HER-2过表达型乳腺癌,患者绝经情况可作为乳腺癌的风险因子,但对乳腺癌分子分型的影响目前尚无明确定论。本研究结果显示,Luminal B型乳腺癌患者的腋窝淋巴结转移率高于其他3种乳腺癌,但王琰娟等[5]认为TNBC和HER-2过表达型乳腺癌淋巴结转移率高于Luminal A型与Luminal B型乳腺癌,这与本研究结果不一致,这种差异可能与研究对象、研究环境的不同有关。黄秒等[6]的研究结果显示,腋窝淋巴结转移阳性提示HER-2表达阳性可能,这在一定程度上提示Luminal B型、HER-2过表达型乳腺癌的可能。方琦和王旭芬[7]的研究结果显示,HER-2可通过促进酶类分泌,从而提高细胞的运动能力,加快肿瘤侵袭及转移的能力。
超声检查是目前重要的乳腺癌检查方法之一[8]。康佳等[9]的研究结果显示,不同分子分型的乳腺癌形态多表现为不规则形,这可能与研究的病理类型多数为浸润性乳腺癌有关,肿瘤向周围组织浸润生长,引起周围纤维结缔组织反应。Luminal A型乳腺癌肿瘤边缘多表现为模糊、成角或毛刺征,以Luminal B型和HER-2过表达型乳腺癌多见。孙斌等[10]的研究结果显示,雌激素受体(ER)表达与病灶边缘模糊及病灶边缘成角呈正相关。而Wang等[11]认为HER-2基因的表达与边缘毛刺征具有正相关性。TNBC的生长模式倾向于快速增殖,肿瘤细胞常呈推挤式增生,因此边缘易形成分叶状[12]。Luminal B型和HER-2过表达型乳腺癌肿瘤内血流信号较丰富,Alder分级主要为Ⅱ或Ⅲ级。Wang等[13]的研究结果显示,HER-2基因与血管内皮生长因子的表达相关,HER-2基因使血管内皮细胞增殖,促进血管生成,新生血管数目多,缺乏肌层,故血流信号丰富,进而使肿瘤生长、侵袭、转移。Hasan等[14]的研究结果显示,Luminal B型乳腺癌血流信号丰富可能与Ki-67高表达或HER-2表达阳性有关。Ki-67是一种增殖细胞抗原,与细胞有丝分裂密切相关,是乳腺癌预后的重要标志物,其高表达促进细胞活跃增殖,故而需要丰富的血流,使肿瘤快速生长[15]。
MRI检查具有较高的软组织分辨力,可以提供病灶形态学特征、血流动力学及血管生成等多参数信息,是检测乳腺癌的灵敏方法[16]。我们发现Luminal A型、Luminal B型和HER-2过表达型乳腺癌多表现为不均匀强化,TNBC在MRI强化特征中多表现为环形强化。MRI强化程度主要由肿瘤组织的血管密度及对比剂进入肿瘤组织的数量决定。毛锡金等[17]的研究结果显示,TNBC边缘区域微血管密度高,肿瘤生长较快,中心区域血流较少,中心易坏死。而HER-2和Ki-67的高表达促进大量的新生血管生长,进而使肿瘤生长加快,血流分布不规则,使Luminal B型和HER-2过表达型乳腺癌肿瘤的强化特征表现为不均匀强化。
乳腺X射线摄影检查作为诊断乳腺癌常用的检查方法之一,可提供乳腺癌形态、密度、边界、钙化等重要信息。HER-2过表达型和Luminal B型乳腺癌的钙化率高于Luminal A型和TNBC,HER-2过表达型乳腺癌肿瘤钙化形态多以细小多形性及线样为主,Luminal A型多为点状钙化,这与胡仰玲等[18]的研究结果一致。肿瘤钙化与肿瘤坏死产物、肿瘤自主分泌的代谢产物或钙盐沉积有关,Cai等[19]的研究结果显示,HER-2基因具有促进肿瘤钙化的作用。雌激素受体(ER)与HER-2基因可能参与钙离子的转运过程,但目前尚无明确定论[6]。
综上所述,不同分子分型乳腺癌的临床特征及治疗方案存在较大差异,乳腺癌肿瘤边缘和患者绝经情况可作为乳腺癌分子分型的独立预测因子。超声、MRI及乳腺X射线摄影检查作为筛查乳腺癌无创且易行的影像检查方法各有优势,不同分子分型的乳腺癌在不同影像特征上具有一定的差异性。不同检查技术的联合将有助于提高乳腺癌分子分型诊断的准确性。
利益冲突 所有作者声明无利益冲突
作者贡献声明 刘晓瑜负责研究命题的设计与提出、数据的校对、论文的撰写与修改、研究过程的实施、数据的收集与统计分析;林翠君负责研究过程的实施、图像的校对与审阅;黄洁负责研究过程的实施、数据的收集与统计分析;代海洋负责研究命题的设计与提出、数据的校对、论文的审阅与修订
Diagnostic value of ultrasonography, MRI and mammography features of breast cancer with different molecular types
- Received Date: 2022-12-26
- Available Online: 2024-02-25
Abstract:









 DownLoad:
DownLoad: